Improved Ocular Disease Diagnosis by UWF Retinal Imaging of Peripheral Vascular Abnormalities
Ultra-widefield (UWF™) retinal imaging of vascular abnormalities in the retinal periphery is improving the diagnosis of ocular disease.
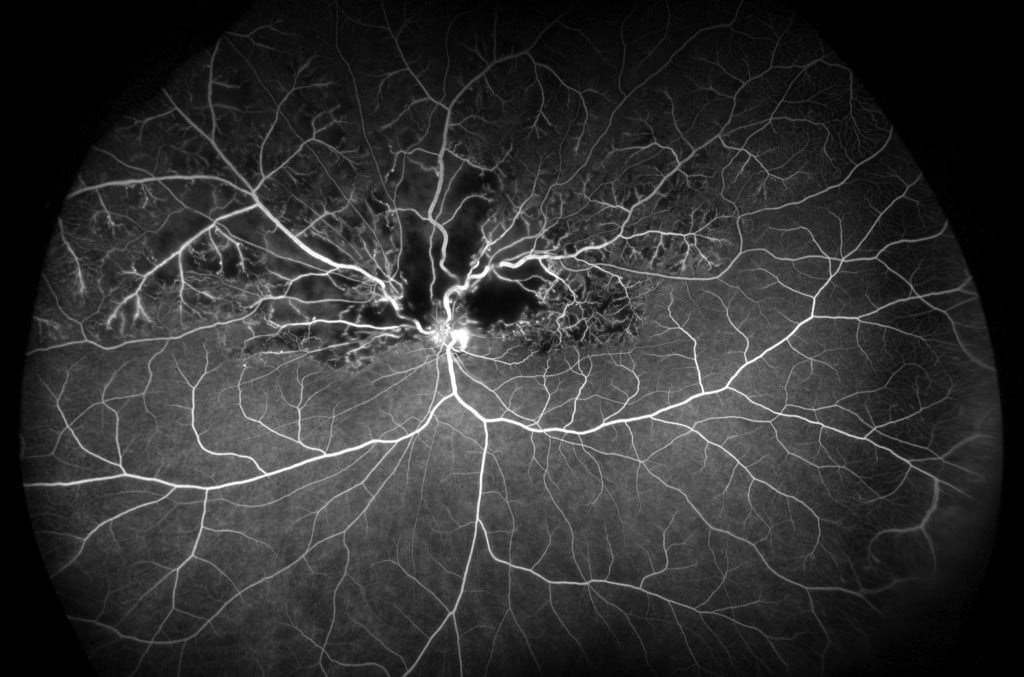
Hemi Retinal Vein Occlusion FA, California
While retinal vascular abnormalities are part of the pathology of many ocular diseases, conventional retinal imaging is unable to inform practitioners about the extent to which these vascular abnormalities are present in the retinal periphery. A growing body of research and case studies using UWF imaging is demonstrating that characterization of vascular abnormalities of the retinal periphery can contribute to and improve the diagnostic process.
About Ultra-Widefield Retinal Imaging
UWF retinal imaging is performed by a specially designed scanning laser ophthalmoscope (SLO) that generates a high-resolution digital image covering 200° (or about 82%) of the retina. By comparison, conventional 7 standard field (7SF) ETDRS and fundus camera photographs produce a relatively narrow view (60° or less) of the retina.
The devices simultaneously scans the retina using two low-power lasers (red and green) that enable high-resolution, color imaging of retinal substructures. The resulting UWF digital image – the optomap – is produced in a single capture. Along with UWF color imaging, the technology supports UWF fluorescein angiography (FA), UWF fundus autofluorescence (FAF), and UWF indocyanine green angiography (ICG).
Peripheral Vascular Abnormalities – General Findings
A retrospective, observational study, Peripheral Vascular Abnormalities Identified With Ultra-Widefield Fluorescein Angiography: Findings of Widefield Angiography Leading to Revised Diagnosis of Retinal Vascular Disease, reviewed the UWF FA images of 284 patients diagnosed with diabetic retinopathy (DR), uveitis, Coats’ disease, retinopathy of prematurity and several other ocular diseases. Of these patients, 11% were found to have vascular abnormalities in the retinal periphery that impacted the patients’ diagnoses. In particular, peripheral neovascularization was found in 18% of patients with DR. Peripheral vascular leakage was found in patients with uveitis and retinopathy of prematurity, and temporal ischemia in patients with Coats’ disease.
While these results aren’t statistically significant across all patients, they indicate how peripheral retinal vascular abnormalities can impact individual diagnoses.
More Comprehensive Diabetic Retinopathy Diagnosis
Another study, Ultra-widefield Angiography Improves the Detection and Classification of Diabetic Retinopathy, focused exclusively on patients with DR and found that UWF FA imagery uncovered significantly more vascular abnormalities than conventional standard field (7SF) imaging. Imaging 218 eyes, UWF imaging visualized 3.9 times the areas of nonperfusion and 1.9 times the area of neovascularization. In 10% of patients, vascular abnormalities (including neovascularization and nonperfusion), were identified that otherwise were not evident in 7SF images.
Peripheral Vascular Abnormalities in Uveitis
Uveitis, associated with several ocular diseases, requires special diagnostic emphasis that can benefit from UWF imaging. A study undertaking a retrospective review1 of several illustrative uveitis cases, Role of Ultra-Widefield Fluorescein Angiography in the Management of Uveitis, found instances in which UWF fluorescein angiography identified peripheral retinal vasculitis, areas of poor perfusion, and active peripheral phlebitis that would not have been identified using conventional, narrowfield 7SF imaging.
The evidence suggests that this additional information can have a significant impact on treatment decisions. In another study2, Wide-field Retinal Imaging in the Management of Noninfectious Posterior Uveitis, physicians changed patient management decisions in 48% of the non-infectious uveitis cases where scanning laser ophthalmoscope images and UWF FA were included in the diagnostic work-up.
Peripheral Retinal Nonperfusion in Retinal Vein Occlusion (RVO)
Central and Branch RVO present diagnostic complexities and patient management may be marked by recurrent macular edema requiring one or more follow-on treatments. A study3, Area of Peripheral Retinal Nonperfusion and Treatment Response in Branch and Central Retinal Vein Occlusion, examining 32 patients with recurrent macular edema used UWF FA to characterize areas of retinal nonperfusion over the course of their continuing treatment. While the study’s authors found no relationship between the extent of ischemia and response to treatment, increased areas of ischemia were associated with more severe instances of recurring macular edema. The study’s authors observed that patients with severe macular edema might be candidates for UWF FA imaging in order to identify any peripheral nonperfusion and/or possible neovascular complications.
Vascular Abnormalities in Central Serious Chorioretinopathy (CSC)
Using a different UWF imaging modality, clinicians reported4 on their use of UWF indocyanine green chorioangiography in their treatment of a group of patients with CSC. While using UWF fundus autofluorescence to assess the health of their patients’ retinal pigment epithelium, UWF ICG images were obtained from a subset of patients (24 eyes), to characterize choroid circulatory function.
Early phase UWF ICG imagery showed that most eyes (83%), had indications of outflow congestion of draining vortex veins as suggested by dilated choroidal vessels extending back to one or more vortex vein ampullas (the authors suggested that relating the severity of this outflow congestion to the severity of CSC symptoms is an area for further research).
In one patient, UWF ICG imaging identified areas of choroidal hyperpermeability. These areas were targeted with reduced verteporfin photodynamic therapy with good results and complete resolution of the associated macular sub-retinal fluid.
******
The most important common theme in these studies is that the diagnosis of some of the most common ocular diseases can be improved by fully characterizing related vascular abnormalities in the peripheral retina. UWF retinal imaging is playing an expanding role in the diagnosis, management, and treatment of these diseases, and as research on the role of peripheral vascular abnormalities continues there will be further developments that will improve patient outcomes.

Sources:
- Hong BK, Khanamiri HN, Rao NA. Role of ultra-widefield fluorescein angiography in the management of uveitis. Can J Ophthalmol. 2013;48:489-493.
- Campbell JP,Leder HA,Sepah YJ,etal. Wide-field retinal imaging in the management of noninfectious posterior uveitis. Am J Ophthalmol. 2012;154:908-11.
- Singer M, Tan CS, Bell D, et al. Area of peripheral retinal nonperfusion and treatment response in branch and central retinal vein occlusion. Retina. 2014;34(9):1736-1742.
- Pang CE, Shah VP, Sarraf D, Freund KB, Ultra-Widefield Imaging with Autofluorescence and Indocyanine Green Angiography in Central Serous Chorioretinopathy, American Journal of Ophthalmology (2014), doi: 10.1016/j.ajo.2014.04.021