A New Look at Non-proliferative Diabetic Retinopathy
One of the ways to measure the impact of a diagnostic technology is its ability to reveal insights into the origins and progression of disease. A recent study1 using ultra-widefield (UWF™) imaging is providing researchers and practitioners with a new look at diabetic retinopathy (DR). It suggests a novel way to characterize DR that may lead to a better understanding of where and how it develops.
Diabetic Retinopathy and Ultra-widefield Imaging
Over the past decade, UWF imaging has become an important tool in the assessment and treatment of DR. UWF optomap® color imaging, performed without pupil dilation, is recognized as providing diagnostic accuracy equal to the gold standard, ETDRS seven-field color fundus photography (7SF)2. Similar results have been documented for UWF fluorescein angiography, or optomap fa. Studies using optomap fa uncovered significantly more retinal vascular pathology in DR patients as compared to 7SF imaging.3
Both optomap and optomap fa give the practitioner a 200° view of the retina – a significant improvement of the 90° view afforded by 7SF imaging. This wider view of the peripheral retina has created an opportunity to develop a more complete picture of how DR develops and progresses.
Definitions and Methods
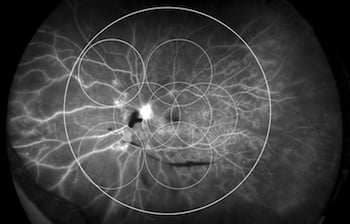
The core question posed by the study was whether the location of diabetic lesions in the retina could be of clinical significance. The study’s authors defined “anterior” diabetic retinopathy as being DR found entirely outside of a circle superimposed over the seven standard ETDRS fields. (See Figure 1.) Patients with DR entirely inside the 7SF circle were classified with “posterior” DR, and those with DR in and out of the circle were classified with “diffuse” DR.
The study’s subjects were hospital-based patients with non-proliferative diabetic retinopathy (NPDR). Individuals with non-diabetic pathology or with conditions that would compromise evaluation of their angiograms were excluded. Subjects were examined using both optomap fa and traditional fundus images. The severity of their NPDR was classified per ETDRS definitions. Other data collected included patient histories, use of insulin and other medications, and a spectrum of blood work consistent in studies of this type. One eye was chosen for analysis from each of the 234 participants.
Findings and Discussion
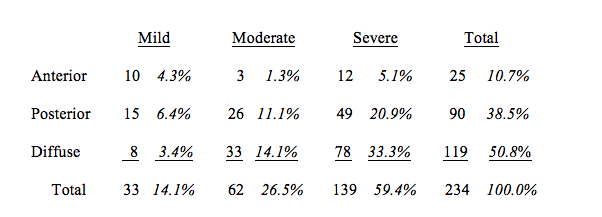
The proportion of the study population with anterior NPDR totaled 10.7%. Posterior NPDR was 38.5% of the group and diffuse NPDR the remaining 50.8%. (See table, below.)
The authors also found that:
— Anterior NPDR was statistically higher in less severe stages of NPDR.
— Anterior NPDR was statistically correlated with low HbA1c levels, high HDL-C levels, and the use of lipid-lowering agents.
— No statistical correlation was found between the location of NPDR and diabetes duration.
One of the important findings of this study is the characterization of a small, but significant, class of DR that is undetectable using standard ETDRS seven-field color fundus photography. This illustrates how UWF imaging can improve the DR screening and diagnostic process. The authors, noting the almost 11% rate of anterior DR in their select group of hospital patients, speculated that the rate in the general diabetic population may be even higher.
Stage of NPDR and Location
(number of eyes – percentage)
Some of the study’s findings raised questions that could lead to valuable paths for future research:
— According to the authors, the correlation between anterior DR and less severe stages of NPDR might be caused by the tendency of more severe cases to progress into diffuse DR. Alternatively, rapidly progressing DR might be more likely to present as posterior or diffuse.
— While anterior DR was correlated with good Hb1Ac and HDL-C control, the authors were cautious about the implications. Past studies linking good blood sugar and lipid control with reduced risk of DR progression did not examine the peripheral retina. The authors suggested that where these past studies may have classified a case as without DR, in fact, anterior DR might have been present.
—The inability to correlate the location of DR to diabetes duration may be significant. The authors put forward that this might be evidence that diabetic patients have a predetermined DR development point, and that DR would first present as anterior DR in cases where blood sugar and lipids are under good control.
The authors, careful to point out the limitations of their small-scale study, have nonetheless suggested a new way to think about DR. Using UWF imaging, researchers may be able to use the location of DR pathology to build a more complete understanding of DR progression. In turn, that could lead to better strategies for diagnosis and treatment.
About optomap and Ultra-widefield Retinal Imaging
UWF imaging technology gives ocular health practitioners imagery and diagnostic information about the retinal periphery that can’t be provided by small-field imaging methods. UWF retinal imaging technology from Optos is a multi-modal platform which supports color optomap, fundus autofluorescence (optomap af), fluorescein angiography (optomap fa) and indocyanine green angiography (optomap icg) providing customizable solutions for use in multiple eyecare settings.

Sources:
- Bae K, Lee JY, Kim TH, Cho GE, et al, Anterior Diabetic Retinopathy Studied by Ultra-widefield Angiography, Korean J Ophthalmol. 2016 Oct;30(5):344-351. Epub 2016 Sep 29.
- Silva PS, Cavallerano JD, Sun JK, Noble J, Aiello LM, Aiello LP, Nonmydriatic Ultrawide Field Retinal Imaging Compared with Dilated Standard 7-Field 35-mm Photography and Retinal Specialist Examination for Evaluation of Diabetic Retinopathy, American Journal of Ophthalmology, May 2012
- Wessel MM, Aaker GD, Parlitsis G, et al. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina 2012;32:785-91.