UWF Imaging Supports Early Diagnosis of Dry Age-related Macular Degeneration
Age-related macular degeneration (AMD) is one of the world’s leading causes of central vision loss in industrial nations, causing significant visual morbidity. Non-exudative AMD accounts for approximately 90% of all reported cases.
There is a growing body of evidence suggesting that there may be early indicators preceding the development of AMD. Over 30 years ago, while investigating reticular degeneration of the pigment epithelium (RDPE), Lewis et al, discovered a correlation between the characteristics of macular degenerative changes and RDPE. One of their recommendations supported the value of observing the peripheral retina, when assessing patients with macular degenerative abnormalities1.
Understanding the relevance of peripheral retinal abnormalities, to disease progression relating to AMD and other retinal conditions, continues to evidence the value of ultra-widefield (UWF™) imaging in this process. In the 12-year follow-up of subjects from the Reykjavik Eye Study, Lengyel et al2 evaluated subjects using optomap® color and autofluorescence (AF) imaging.
The peripheral retina was phenotyped using categories defined in the International Classification of AMD which was developed to characterize the macula. The population sample was 576 subjects. Of the eyes examined, 81.1% had AMD-like changes in the macula. From this sample, 13.6% of subjects were noted to have AMD-like changes in the macula alone, 10.1% in the periphery alone, and 57.4% of subjects in both periphery and macula. UWF (up to 200°) color and autofluorescence images were obtained using the Optos laser scanning ophthalmoscope (Optos plc, Dunfermline, Scotland). Authors concluded that the International Classification scale should be reevaluated to include these pan-retinal changes.
In the Optos Peripheral Retina (OPERA) study, conducted in Croatia3, Friberg et al, found a significant relationship between the presence of peripheral reticular pigmentation (PREP) and the presence of AMD.
In the Croatian OPERA study, 150 subjects with AMD, in one or both eyes, had both eyes imaged with UWF. Both ultra-widefield fluorescein angiography (UWF-FA) and color images were taken. AMD was defined according to the International ARM (Age-related maculopathy) Study guidelines. The control group contained 150 matched subjects without AMD, who were photographed in a similar way, but without angiography. Masked readers identified the presence or absence of PREP for all study subjects, making note of the number of quadrants of pigmentation in each eye. Other morphological parameters were noted, which included drusen, paving stone degeneration, white-without pressure, and lattice degeneration.
Findings demonstrated the presence of PREP in 8.1% of control eyes compared to 40.6% of eyes in subjects with AMD. UWF-FA increased the sensitivity of the assessment of PREP where it was found in 46.3% of eyes in subjects with AMD. Authors identified a strong correlation between subjects with AMD and those presenting with PREP.
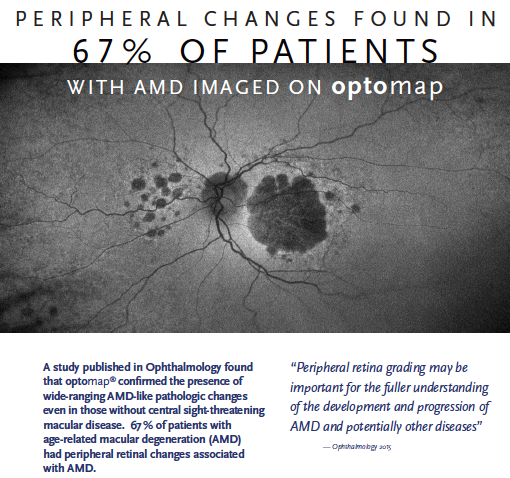
The recent use of UWF imaging in an Age-Related Macular Degeneration Study 2 (AREDS2) sub-study OPERA4, included 484 subjects who were imaged with color and AF UWF. It was observed that peripheral retinal changes were more prevalent (97%) in eyes that have AMD in comparison to the control group, further supports previous indications. In this study, Domalpally et al submit, “Age-related macular degeneration may be more than a “macular” condition but one that involves the entire retina.” The authors of the study encourage further investigation in to this finding and are beginning a longitudinal study using Optos UWF imaging for peripheral retinal assessment in AMD subjects.
For patients who are identified as predisposed to developing AMD, the integration of optomap imaging has the potential to be an invaluable clinical workflow technology to support the early detection of peripheral changes, map disease trajectories, engage patients with a visual representation of real time images of their eyes, and give them an opportunity to become more invested in their eye health, with the ultimate goal of sight preservation.
Sources:
- Hilel Lewis. MD, Bradley R. Straatsma.MD, Robert Y. Foos. MD , David O. Lightfoot. (1985) Reticular Degeneration of the Pigment Volume 92, Issue 11, November 1985, Pages 1485-1495 Ophthalmology
- Lengyel I, Csutak A, Florea D, Leung I, Bird AC, Jonasson F, Peto T.(2015) A Population-Based Ultra-Widefield Digital Image Grading Study for Age-Related Macular Degeneration-Like Lesions at the Peripheral Retina. Ophthalmology. 2015 Jul;122(7):1340-7. doi: 10.1016/j.ophtha.2015.03.005. Epub 2015 Apr 11.
- Vesna Jurisic Friberg, Biljana Andrijevic Derk , Tamara Kenezevic, Mia-Zoric-Geber, Goran Bencic, Zoran Vatavuk, Thomas R. Friberg.(2013) OPERA (Optos Peripheral Retina AMD) Study in Croatia: Reticular Pigmentation in Age-Related Macular Degeneration vs. Control Methods. University Department of Ophthalmology – Zagreb Croatia, University of Sarajevo, UPMC Eye Center Pittsburgh USA.
- Amitha Domalpally, MD, Traci E. Clemons, PhD, Ronald P. Danis, MD SriniVasR.Sadda, MD Catherine A. Cukras, MD, PhD Cynthia A. Toth, MD Thomas R. Friberg, MD Emily Y. Chew, MD (2017) Peripheral Retinal Changes Associated withAge-Related Macular Degeneration in the Age-Related Eye Disease Study 2 Age-Related Eye Disease Study 2 Report Number 12 by the Age-Related Eye Disease Study 2 Optos PEripheral RetinA (OPERA) Study Research Group∗