Ultra-widefield (UWF™) optomap® technology sets a new standard for early detection and diagnosis by providing a wider view of the retina coupled with superior imaging capabilities.
“If you are not looking at the peripheral retina, you don’t have the whole picture, and you are not able to adequately assess risk. This is why we need to look at everybody and see what is out there.” Dr Jeffry Gerson
optomap – Illuminating a Wider Landscape
optomap imaging reveals an expansive view of the retinal landscape, exposing issues otherwise left undiscovered and untreated. Increasing utilization of UWF technology is also changing the landscape of ocular health care.
Unlike exploration prompted by patient reports of symptoms or history of retinal problems, optomap imaging captures a high resolution, 200° digital image of the peripheral retina in addition to the central pole in a single dynamic image.
Dr. Jeffry Gerson of Grin Eye Care in Kansas City adopted optomap early and has observed firsthand the evolution of the technology over 13 years. Gerson recognized the value of UWF optomap imaging immediately. Today, he says he cannot imagine practicing without it.
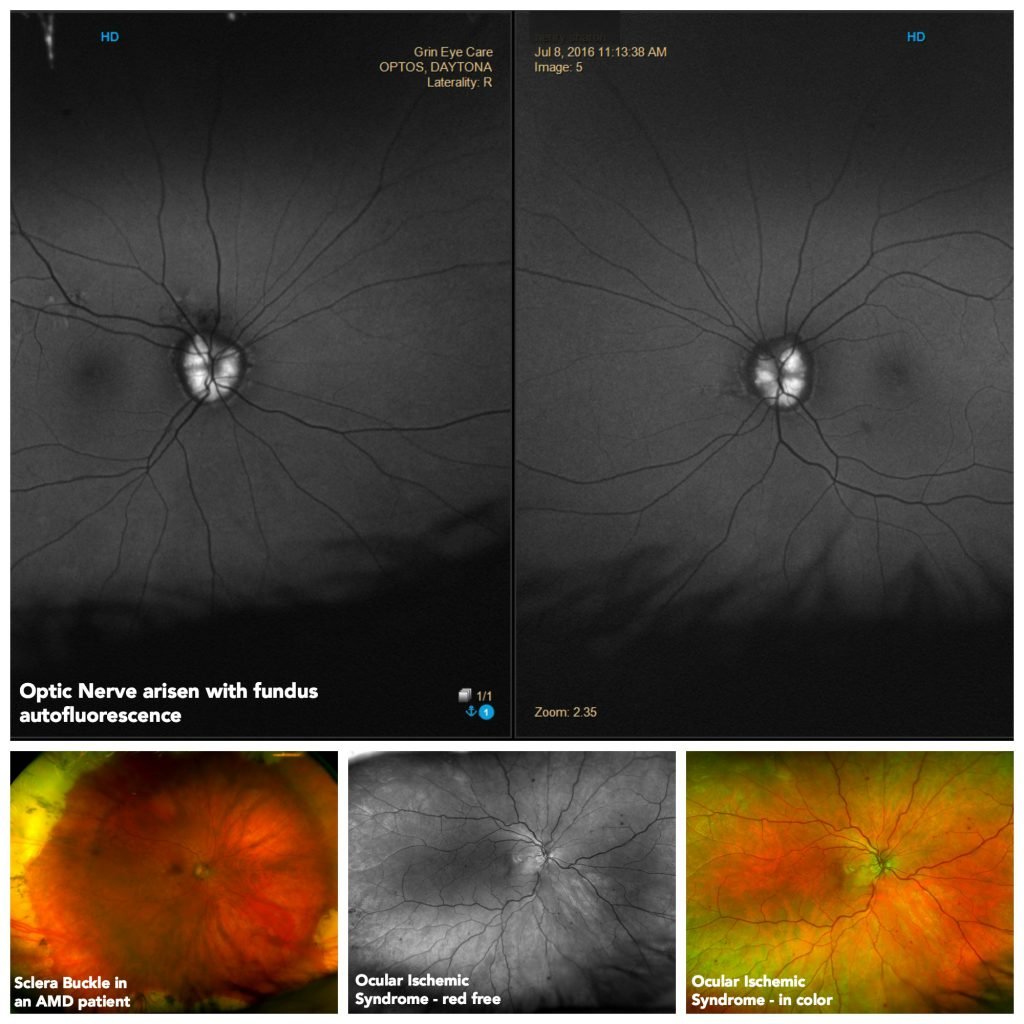
Images captured by Dr. Gerson with his optomap device.
“Initially it impacted how I practiced. Because of an increase in pathology, I was suddenly able to identify what I did not expect to see, or otherwise would not have seen.”
optomap is a valuable resource for the identification and treatment of peripheral retinal breaks, risk assessment in diabetes, and understanding of the association between the peripheral retina and macular pathology.
Before optomap, patient symptom reports largely directed the discovery of peripheral pathology – optometrists performed advanced testing only when warranted by reports of symptoms or history. Delays in testing could allow further progression of serious pathologies, such as peripheral retinal breaks.
“However,” Gerson notes that while using optomap, “we discover peripheral pathology frequently in patients who are completely asymptomatic.”
optomap gives optometrists an opportunity to observe and assess diabetic risk or severity of diabetic retinopathy before the subtle signs of peripheral retinopathy develop. This is particularly important because, in many cases, the peripheral retina corresponds with macular pathology. Without a view of the peripheral retina, however, optometrists cannot adequately assess risk.
“If you are not looking at the peripheral retina, you don’t have the whole picture, and you are not able to adequately assess risk. This is why we need to look at everybody and see what is out there.”
Once a noteworthy event at his practice, Gerson notes the consistent discovery of peripheral pathology and the early detection of disease in the periphery at his practice is now relatively normal.
“This aspect – that I will find what would be otherwise obscured pathology – no longer surprises me.”
Despite the now-routine discovery of pathologies that were once just outside the scope of imaging, advances in optomap technology continue to enhance the practice of Gerson and other optometrists.
“Over the years I have witnessed the updates and upgrades as well as the advances in image quality. I believe initially one of the big concerns for practitioners was image quality. That issue really doesn’t exist anymore. The image resolution is excellent.”
Illuminating Patient Education
optomap helps optometrists inspire patients to take an active role in their own care. Showing a patient their optomap image containing a clear image of disease progression creates a much stronger impression than merely telling patients about the problem. Patients appreciate the quality of the images they see, and they respond positively to the visual information.
Gerson notes that fundus autofluorescence (FAF) imaging has a similar positive effect on patient education in cases where color images do not adequately capture compelling evidence of disease progression. FAF images help patients with retinitis pigmentosa see the progression of their disease, for example.
Autofluorescence (AF) is also helpful in cases of dry AMD, particularly in the advanced stages of geographic atrophy (GA). In these cases, AF detects hyper- and hypofluorescence that indicates whether the disease is active or stable. optomap autofluorescence images help optometrists identify peripheral changes that prompt further investigation of the macula.
Gerson describes the process of grasping the immense potential and importance of utilizing all the functions available with optomap technology as an “evolving mindset,” one in which practitioners progress past simply obtaining a UWF color image; they begin to harness the power of red-green separations and AF to create a comprehensive picture of a patient’s ocular health.
***
About Jeffry D. Gerson
Jeffry D. Gerson, O.D., F.A.A.O., is a practicing optometrist as well as a writer and lecturer on retinal disease management. After graduation from Indiana University School of Optometry in 1997 and completion of his residency at the VA Medical Center in Kansas City, Gerson joined the faculty at the University of Kansas School of Medicine.
Gerson is a member of American Optometric Association and Kansas Optometric Association and is a fellow of Academy of Optometry and Optometric Retina Society. Dr. Gerson serves on numerous advisory boards and is widely considered a thought leader in the management of retinal disease.
