Athletes of all levels need to protect themselves from injury. Injuries are unfortunately a part of playing sports – anyone from weekend warriors to professionals, has probably nursed some sort of injury. In some cases, these injuries happen directly to the eye, from orbital blowout fracture, ruptured globe, or a detached retina and some can be detected, along with other types of ocular and systemic pathology, by looking at the health of the eye.
Both retinal trauma and detachments are not uncommon in sports-related injury. Utilizing optomap during detection and treatment can be particularly useful.
There have been, and continue to be, many studies in the area of sports-related eye trauma. And with more and more interest in the effects of concussions on athletes, seeing “inside” the eye is becoming increasingly important. An x-ray, MRI, CT scan will tell you if something is broken and may confirm a diagnosis of concussion. But what about the effects of repetitive concussive injury? Can that be detected by imaging the eye itself? According to the Centers for Disease Control, up to 3.8 million sports-related concussions occur each year. And detecting these injuries is not always straightforward or based exclusively on objective signs and symptoms. Or what about treating the whole athlete and monitoring systemic as well as ocular health?
Because the retina is the only place in the body where vasculature can be viewed non-invasively, eyecare professionals are looking to the retina to assist them in identifying, diagnosing, and treating ocular and systemic disease in athletes. With the addition of advanced eye testing, in some cases, ground-breaking discoveries have been made on diseases that have only been able to be identified posthumously, such as chronic traumatic encephalopathy1.
Using retinal images to ascertain overall athlete health is also important. Using images, such as optomap ultra-widefield retinal images, can assist detection of systemic disease as well as ocular disease.
Focus on Sports Vision
What makes a doctor decide to focus on sports vision as a specialty? In a recent interview with Dr. Bronson Hamada of Surf City Optometry of Huntington Beach, CA he explains how he came to his decision to dedicate himself and his practice to the specialty of sports vision.
Tell us more about your passion for helping athletes reach their full human athletic potential. Why did you decide to specialize in athletes?
As a collegiate athlete, I had Olympic aspirations, but I thought that being a competitive athlete and pursuing a professional degree were mutually exclusive pursuits. So I chose optometry, not knowing that there was a way to combine my passion for sports with professional eye care. In other words, I thought I’d be spinning dials and selling eyeglasses, but now I handle visual performance for several US National Teams, universities, and a host of professional athletes. I am dedicated to helping athletes of all levels achieve their athletic goals by helping them see better and by training them to use their eyes more effectively.
However, when focusing on these elite athletes it is imperative to remember that they use their eyes differently than recreational athletes. I consider sports vision training to be applied vision therapy, so we’ve gone full circle; back to the basics. It’s the same fundamental vision skills, but the patient is now in motion and processing multiple tasks and facing a dynamic, interactive playing field. The good news for our profession is that coaches, trainers, and athletes are seeking our specialized services – athletes to gain even a slight advantage and coaches and trainers for general eye health and athlete investment.
How do you treat ocular and systemic disease and pathology with your innovative eyecare solutions as part of your comprehensive vision test for athletes?
We are always mindful of their goals, health and personal issues, and motivation. I look at each athlete holistically, without judgement, and work to earn their trust. It is important to remember that ocular and systemic disease can affect anyone, and athletes are no different. Training and competing with those afflictions can be a challenge at any level. One of our athletes that recently retired from international competition had Sjogren’s Syndrome and Lupus.
Here is an example of an innovative eye care solution for an Olympic Champion that suffered a traumatic eye injury. This is an excerpt from an email he sent, “I had a big facial injury and reconstructive surgery and now I am having some vision impairment. There were six facial fractures in total. I will be here (Russia) this entire week and then on to the World Cup (Japan) for Olympic qualification. I am recovering and playing and seeing some vision impairment that is intimidating and affecting my performance…ready to aggressively try and fix it. Hope you are up for it.”
We compared baseline and post traumatic vision assessments and looked for opportunities where we could make the biggest impact. We evaluated ocular health (including retinal evaluation) and eye function and then developed a sports vision training plan with less than one week before World Cup. I had no idea what kind of shape he would be in when he arrived, so I concentrated on eye-hand coordination, timing, eye tracking with smooth pursuit and saccadic eye movements, central and peripheral vision, and depth perception, among other treatments. Next we loaded the skills training with strobe glasses. Within a few days, his vision skills improved – more importantly, he gained confidence. We put together a vision training kit for him to take on the road. Later that season, his professional team in Russia won the Champions League Finals, and he represented Team USA at the London Olympics.
How does optomap fit into your treatment plan?
We had a complete paradigm shift! Our initial thought was that optomap was a shiny, nice-to-have, device but we were concerned that our patients would balk at the extra fee. My staff believes in the technology, presents it with enthusiasm and this translates into a tremendous capture rate that helps our bottomline. Many patients avoid routine eye care simply because they dread the dilating drops and don’t want to be “visually impaired” for 3+ hours. Very quickly we began to appreciate the power of optomap for pathology detection and management. optomap is now an indispensable technology, and I can’t imagine practicing without it. I consider optomap the new “Gold Standard” of care for retina evaluation of athletes. We have greater patient satisfaction, save valuable clinical time, generate referrals, and have peace of mind in knowing that we didn’t miss anything.
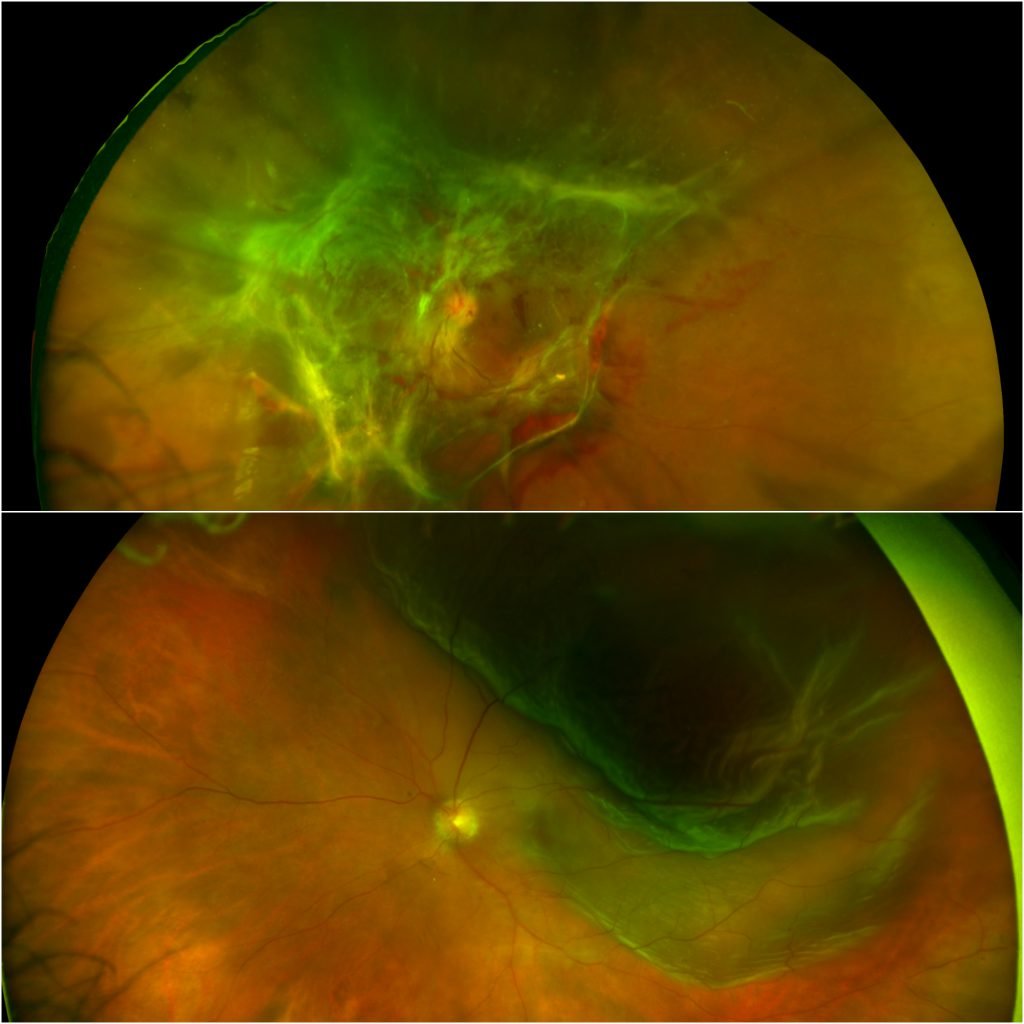
In addition, the very first day the device was installed, we had a professional athlete that got hit in the face with a ball during practice. The optomap revealed peripheral retinal hemorrhages. Talk about a shift!
In another case, an athlete had an “8 Ball” hyphema and received hydrocortisone IV, and retinal surgery while hospitalized in Germany. With optomap, I am able to get an extensive view of the retina before even stepping into the exam room to monitor and treat any ongoing pathology and determine overall eye health.
Do you consult with other doctors in the area to offer a comprehensive line of care for these athletes?
There are many pieces to the athletic performance puzzle. Optometry and sports vision care are definitely multidisciplinary, so a referral network of trusted specialists is crucial. With athletes of any ability, it is inevitable that as a healthcare provider you will encounter TBI, concussion, and ocular injury. Unfortunately, we see high school athletes that have suffered multiple concussions. Coaches and trainers rely heavily on our judgement for “return to play” decisions. So the more information we have, the better the recommendation we can make. Any significant anterior segment injury can have posterior segment consequences.
Many of the athletes that I care for are extremely tall. Cardiologists and geneticists refer several athletes every year to rule out Marfan’s Syndrome2. This systemic disease can have fatal consequences. Some of the lesser known ocular manifestations of Marfan’s Syndrome are strabismus, myopia, glaucoma, retinal tears, and retinal detachment, so optomap is routinely ordered. Optos devices have been used in the clinical environment for detection of retinal pathology specifically for Marfan’s Syndrome.
For doctors such as Dr. Hamada, focusing on sports vision, and working with a team of specialists for overall athlete health and wellbeing, has been quite rewarding. By incorporating technology such as optomap, he and the entire team at Surf City Optometry, are also able to see more and treat more of the retina, thereby providing an even higher standard of care.

References:
- https://www.omicsonline.org/open-access/retinal-and-balance-changes-based-on-concussion-history-a-study-of-division-football-players-2329-9096.1000234.php?aid=31804
- Retinal Disease in Marfan Syndrome: From the Marfan Eye Consortium of Chicago Safa Rahmani, MD; Alice T. Lyon, MD; Amani A. Fawzi, MD; Irene H. Maumenee, MD; Marilyn B. Mets, MD